Part 1 : Autism-like Symptoms in 3-Year-Olds: Alternate Diagnoses and Interventions
Case Examples: Autism-like Symptoms with Other Diagnoses
Not all toddlers who show autism-like behaviors (e.g. no speech, not responding to name, not following commands) are ultimately autistic. Below are case reports and conditions where 3-year-old children exhibited such symptoms but were diagnosed with other conditions, along with how they were distinguished from autism and treated:
Developmental Speech Delay (Late Talker) vs. Autism
Diagnosis & Symptoms: Some children are simply late in developing speech (sometimes called “late talkers” or Einstein syndrome). They may be non-verbal or use very few words at age 2-3, raising autism concerns. However, these children often have age-appropriate social engagement – for example, they use eye contact, gestures, and play interactively – and their non-verbal communication is intact.
Distinguishing from Autism: In pure speech delay, social reciprocity is normal; the child responds to their name and engages socially, communicating through gestures or sounds even if they lack words. Autism, in contrast, involves social-communication impairments beyond just speech delay. Experts caution that late speech alone is not conclusive proof of autism – most late-talking toddlers do not develop ASD. Clinicians will check that the child can non-verbally follow commands, share interest (pointing, showing objects), and that there are no repetitive, restricted behaviors unique to autism.
Treatment & Outcome: The primary intervention is speech/language therapy to stimulate language development. Parents are coached to read, talk, and engage the child frequently in social communication. If hearing loss is ruled out and only speech is delayed, many of these children catch up over time. For example, researcher Dr. Stephen Camarata notes that many late-talkers simply “work through” the delay and later speak normally. With speech therapy and language-rich preschool environments, these children often improve; their autism-like silent behavior resolves once language kicks in. No autism-specific treatments are needed if the child shows only a speech delay.
Childhood Apraxia of Speech (CAS) vs. Autism
Diagnosis & Symptoms: Childhood apraxia of speech is a motor-speech disorder where a child has difficulty planning and coordinating the movements needed for talking. A 3-year-old with severe apraxia might be non-verbal or extremely hard to understand, which can resemble autism’s language delays. In CAS, the child understands language and wants to communicate, but their speech is unintelligible with inconsistent errors (they might say a word differently each attempt). Parents often report the child uses gestures or sounds to get needs met, but doesn’t develop clear words.
Distinguishing from Autism: The key difference is in social interaction and intention to communicate. A child with apraxia typically has normal social engagement – they make eye contact, respond to name, show objects to others, and use facial expressions appropriately. They are frustrated by their inability to speak, whereas an autistic child might not attempt as much communicative interaction. In one clinical study, specialists suspected some non-verbal children had CAS instead of (or in addition to) autism; careful speech evaluations can confirm apraxia by noting the characteristic speech inconsistencies and prosody errors. If a child is social and uses non-verbal communication normally, but cannot form words, CAS is considered. It’s important to test for both CAS and autism when a child has speech delays, since the two can co-occur but require different therapies.
Treatment & Outcome: Intensive speech therapy focusing on motor planning is the main treatment for apraxia. Therapists use repetition and mouth muscle exercises to help the child learn to form sounds and words. For example, in one case a toddler diagnosed with CAS (and not autism) underwent months of specialized speech therapy and began to speak in short phrases. As speech clarity improved, the autism-like signs (lack of spoken language) resolved. Research shows that making the correct diagnosis is crucial because autism and apraxia have very different interventions. With appropriate speech therapy (often using picture cards or sign language as interim communication), children with CAS can significantly improve their speech over time, confirming that their primary issue was apraxia rather than ASD.
Intellectual Disability (Global Developmental Delay) vs. Autism
Diagnosis & Symptoms: Global developmental delay or intellectual disability (ID) can also lead to autism-like behaviors in a 3-year-old. A child with moderate ID will have cognitive and adaptive skills well below age level, possibly appearing socially “young” for their age. For instance, a case study described a 3–4 year discrepancy between a boy’s functional developmental age and his chronological age, consistent with moderate intellectual disability. Such a child might have limited speech, struggle to follow complex instructions, and play in a simpler, repetitive way – all resembling autism. They might also exhibit frustration behaviors (tantrums, self-talk, or aggression) due to learning challenges.
Distinguishing from Autism: A thorough developmental evaluation can differentiate ID from autism. In the case study, the 9-year-old boy had initially been misdiagnosed with autism at age 4, but further assessment showed no core autism symptoms – he initiated social interactions and had reciprocal (if simple) speech, and showed no stereotyped repetitive behaviors. His main deficits were in cognitive and self-help skills. Tools like the Childhood Autism Rating Scale (CARS) yielded scores in the non-autistic range for this child. Unlike autism, where social-communication skills are distinctly impaired, a child with ID may be socially friendly according to their mental age (for example, interacting appropriately with younger kids or familiar adults). The presence of broad delay across all domains (fine motor, gross motor, social, language) suggests global developmental delay rather than autism’s specific social/communication impairment.
Treatment & Outcome: Once identified, treatment focuses on the child’s developmental needs. Early intervention programs and special education can help improve cognitive, language, and adaptive skills. In the cited case, a brief targeted intervention plan was implemented to teach adaptive behaviors (identifying colors, tying shoelaces, basic social manners). With 1:1 teaching, reinforcement, and practice, the boy made gains in independence and socialization. After intervention, he could perform daily tasks more independently and was noted to be social, talkative, and inquisitive – confirming that autism was misdiagnosed and that his challenges stemmed from intellectual disability. This case highlights that a child with ID can improve with appropriate support, and applying “autism treatments” in such a case may be unhelpful or misdirected. Correct diagnosis ensures the child gets therapies suited to their actual needs.
Selective Mutism (Extreme Anxiety) vs. Autism
Diagnosis & Symptoms: Selective mutism is an anxiety disorder in which a child who is fully capable of speaking consistently fails to speak in certain social situations (like preschool or with strangers). A 3-year-old with selective mutism might appear completely non-verbal and unresponsive at daycare or school – prompting suspicion of autism – yet speak freely and normally at home with parents. Key symptoms include a “frozen” demeanor in anxiety-provoking settings: the child avoids eye contact, may appear blank or shy, and doesn’t respond when teachers ask questions. For example, a selectively mute child might not even say their own name at preschool, but at home they chatter, sing, and use age-appropriate language.
Distinguishing from Autism: The context-dependent nature of the child’s silence is the biggest clue. In autism, communication impairment is present across all settings. In selective mutism, the child’s social behavior is normal in comfortable environments (home, with trusted individuals) and only shuts down in specific social settings. If parents report “my child talks and communicates at home, but not at school,” autism becomes less likely. Also, a selectively mute child, when comfortable, demonstrates normal social reciprocity and language for their age – this contrasts with autistic children, who even at home may have limited social interaction or odd communication. The presence of clear anxiety (fearfulness, clinginess, tantrums due to speaking pressure) further points to mutism. Clinicians note there is no inherent link between selective mutism and autism, though a child could theoretically have both. In practice, a child who is mute due to anxiety will warm up and speak when anxiety lowers, whereas an autistic child typically has communication deficits regardless of mood.
Treatment & Outcome: Treatment focuses on reducing the child’s social anxiety and gradually encouraging speech rather than forcing talking. Strategies include behavioral therapy techniques like graded exposure (starting with nonverbal communication, then whispers, then words as confidence builds) and stimulus fading (the child speaks to a familiar person, then new people are gradually introduced). Parents and teachers are advised to relieve pressure to talk, create a supportive atmosphere, and praise any brave communication attempts. With early intervention, most children overcome selective mutism. For instance, a 3-year-old girl who never spoke at preschool began speaking in a whisper to her teacher after several weeks of gentle encouragement and “buddy” sessions with a friend; over months, her voice grew louder. By focusing on anxiety (sometimes with the help of child-friendly cognitive-behavioral therapy), these children often “unlock” their speech. They were never autistic – once anxiety is treated, their social and communication skills appear typical for their age.
Landau-Kleffner Syndrome (Epileptic Aphasia) vs. Autism
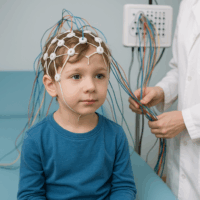
Diagnosis & Symptoms: Landau-Kleffner Syndrome (LKS) is a rare neurological disorder (an epileptic encephalopathy) that can cause a previously typical child to lose language skills and exhibit autistic-like behavior. It usually onsets between ages 3-8. A child with LKS may stop responding to their name and verbal commands, not because of social indifference, but because they develop auditory verbal agnosia – an inability to comprehend spoken language. They often become effectively non-verbal, and this regression can be mistaken for autism or deafness. However, LKS is caused by abnormal brain electrical activity (seizures, often occurring during sleep) damaging language processing areas. For example, a 3½-year-old who had begun talking in short sentences might progressively lose words and appear to withdraw socially, prompting an autism evaluation – when in fact abnormal EEG activity is the culprit.
Distinguishing from Autism: Several features help differentiate LKS from autism. First, the onset is often acute – a child who had normal development suddenly regresses in language over weeks or months, which is atypical for autism (autistic regression usually occurs earlier and not as complete loss of comprehension). Second, children with LKS may show good social interest and play when communication doesn’t require language. Parents might say the child is trying to interact but seems as if they can’t understand or talk. Most critically, an EEG (electroencephalogram) will reveal abnormal epileptic activity in the language areas of the brain, especially during sleep. This is not seen in standard autism. A case report of a child with LKS misdiagnosed as autistic showed that after proper neurological workup, the EEG findings confirmed LKS, explaining the language loss. In contrast to autism, LKS can be considered a medical (neurological) condition producing autistic-like symptoms.
Treatment & Outcome: Early diagnosis is vital because LKS is treatable. The cornerstone is anti-epileptic pharmacotherapy (and sometimes corticosteroids) to control the brain discharges. In one case study, a boy with LKS showed “great improvements” in communication after receiving appropriate medication. Specifically, after intensive anticonvulsant treatment, his responsiveness and speech began to recover, and his Autism Treatment Evaluation Checklist scores improved markedly. Alongside medication, speech therapy and occupational therapy are used to rehabilitate language and social skills. Many LKS children, once treated, regain some or most language ability – a stark contrast to autism, where there is no medication that reverses the condition. This demonstrates that what looked like autism was in fact an epileptic aphasia; suppressing the seizures enabled the child’s development to get back on track. Correctly distinguishing LKS from ASD is critical, as delays in treatment can lead to prolonged language impairment.
Other Conditions Misidentified as Autism
There are a few other conditions that can superficially resemble autism in a toddler, though their core causes differ:
- Reactive Attachment Disorder (RAD): This occurs in children who experienced severe early neglect or trauma, leading to difficulty forming normal social bonds. A 3-year-old with RAD might be withdrawn, avoid eye contact, not seek comfort, and seem indifferent to caregivers – behaviors that overlap with autism. However, if placed in a supportive, nurturing environment, these children can form attachments and show normal social interaction when they feel safe. In contrast, an autistic child’s social difficulties persist even in a loving environment. Key history (neglect/abuse) and the child’s improvement with consistent caregiving point to RAD rather than autism. Therapy for RAD involves stable caregiving and sometimes play therapy to build trust; as the child forms an attachment, their social engagement improves, revealing they were not autistic.
- Severe Sensory Impairments or Other Neurological Issues: (Hearing loss is excluded in this discussion, but worth noting in practice.) For example, severe visual impairment or a motor disability like cerebral palsy might initially mask a child’s social responses (the child may not orient to people typically, or may be limited in interaction), but the underlying issue is sensory/motor, not social understanding. A comprehensive medical evaluation can identify such conditions. Another example is extreme ADHD or OCD in a young child, which can cause unusual behaviors (lining up toys, toe-walking, inattention to name) that mimic some autism signs. The differentiator is that these children do not truly lack social reciprocity – an ADHD child might be impulsively social and an OCD child has anxiety-driven rituals, but neither has the pervasive social communication deficits of autism.
- “Virtual Autism” (Environmental Deprivation): This is a proposed term for autism-like symptoms arising from environmental factors, such as excessive screen time and lack of social interaction in early years. There have been reports of toddlers who had very high exposure to screens (TV, tablets for many hours a day) and developed delayed language and social skills. They might appear non-responsive and engaged in their own world (e.g. fixated on videos) similar to autism. One case report documented a 2-year-old boy who met criteria for ASD, but over a 4-month period without any specific intervention his symptoms resolved. The parents had dramatically reduced his screen exposure during this time. At 28 and 36 months old, he was re-evaluated: he now responded to his name, had typical eye contact, and age-appropriate speech and play, and no longer qualified for an autism diagnosis. This suggests the initial “autism” symptoms were transient and likely due to environmental/social deprivation. In such scenarios, improving the child’s environment – replacing screen time with responsive human interaction and play – can lead to rapid gains. It’s a reminder that developmental history is critical: professionals will ask if the child had opportunities to socialize and communicate; a lack thereof might cause delays that are reversible when conditions change. (Of course, true autism is not caused by bad parenting or screens, but poor environment can cause its own issues.) Once these children receive rich social interaction, they often “catch up,” confirming that autism was not actually present.
Note: A thorough evaluation by specialists (pediatric neurologists, child psychologists, speech therapists, etc.) is essential when a 3-year-old shows autism-like signs. As seen above, conditions ranging from speech apraxia to anxiety or neurological syndromes can sometimes be mistaken for autism. Distinguishing them relies on examining the context and quality of the child’s social responses, any unique medical features (e.g. seizures, trauma history), and testing specific domains (hearing tests, speech motor assessments, etc.). Getting the diagnosis right is crucial, because it directs the child to the proper treatment and gives families a more accurate prognosis.
Part 2 : not bad to mention the Therapies for Diagnosed Autism in 3-Year-Olds (Worldwide Practices)
When a 3-year-old is properly diagnosed with autism, early intervention is key. There are several successful therapies and interventions used around the world to help autistic children develop skills. Below is a structured overview of the most widely used approaches, their goals, and evidence of success (with citations from scientific and clinical sources):
- Applied Behavior Analysis (ABA): ABA is a behavioral therapy that uses principles of learning (reinforcement) to encourage positive behaviors and teach new skills in autistic children. ABA programs for 3-year-olds often involve intensive one-on-one therapy, breaking skills (like language, imitation, following instructions) into small steps and rewarding the child’s successes. For example, Early Start Denver Model (ESDM) is an ABA-based program for toddlers that integrates play and developmental techniques. In a randomized clinical trial, children who received ~20 hours per week of ESDM for 2 years made significantly greater gains in IQ, adaptive skills, and reduction of ASD symptoms compared to those with typical community therapy. Classic ABA research also shows long-term benefits: in the renowned Lovaas study, about 47% of children who got early intensive ABA (40 hrs/week) achieved normal educational functioning by school age. A recent meta-analysis likewise found that comprehensive ABA intervention leads to improvements in cognitive performance, language, and adaptive behavior in many young children with ASD. Overall, ABA is considered an evidence-based treatment for autism. Programs like Discrete Trial Training and Pivotal Response Training are variants of ABA tailored to toddlers, often delivered in homes or preschools. The goal is to reduce problematic behaviors and build communication, social, and self-help skills through repetition and positive reinforcement. ABA’s effectiveness is maximized when started early (ages 2-4) and with high intensity. Many countries have ABA early intervention centers or in-home therapy services to support families.
- Speech and Language Therapy: Since communication deficits are a core feature of autism, speech therapy is one of the most crucial interventions for a non-verbal or minimally verbal 3-year-old. A licensed speech-language pathologist (SLP) works on improving the child’s ability to understand and use language. For a 3-year-old, therapy often focuses on building non-verbal communication first (gestures, pointing, sign language or picture boards) as precursors to words. The SLP will also help the child make sounds, imitate words, and eventually form simple words or sentences. Importantly, speech therapy addresses social communication, not just speech – teaching skills like responding to one’s name, turn-taking in “conversation” (even if non-verbal), and using language for requesting or commenting. In practice, a speech therapist might use play activities to encourage vocalization, or introduce an augmentative communication system (like PECS – Picture Exchange Communication System) so the child can express needs without words. Research and clinical experience show that speech therapy can significantly increase communication in young autistic children – even if speech doesn’t develop immediately, kids often learn to communicate through alternative means which reduces frustration and improves social engagement. Many parent “success stories” cite speech therapy as transformative, with children saying their first words or improving articulation after months of consistent sessions.
- Occupational Therapy (OT): Occupational therapy helps autistic children develop the skills needed for daily life (“occupations” of childhood include playing, dressing, eating, etc.). In 3-year-olds with ASD, OT often focuses on sensory integration difficulties and fine motor skills. Autistic toddlers can be either hypersensitive or under-responsive to sensory input (sounds, touch, textures). An OT uses exercises and sensory activities (e.g. brushing skin, swinging, deep pressure, tactile play) to help the child better regulate their responses to stimuli. This can reduce overwhelm and meltdowns related to sensory issues. Additionally, OTs work on fine-motor and self-care skills: for example, teaching a child how to use utensils, zip a coat, or draw with a crayon – tasks an autistic child may struggle with due to motor planning issues or sensory aversions. They might create play routines that improve hand-eye coordination and body awareness (like obstacle courses for gross motor skills, or puzzles for fine motor). By addressing these areas, OT can improve a child’s comfort in their own body and environment, which often leads to better attention and readiness for learning. Parents often report progress such as a child who previously could not tolerate messy textures now enjoying finger-painting, or gains in independence like being able to wash hands or put on shoes. These functional improvements greatly enhance the child’s quality of life. Occupational therapy, especially when started early, has been shown to help autistic children participate more fully in everyday activities.
- Developmental and Play-Based Therapies (e.g. DIR/Floortime): Unlike ABA’s structured approach, developmental therapies like DIR/Floortime focus on following the child’s lead and using play interactions to foster social and emotional development. In Floortime, the parent or therapist gets down on the floor with the child and engages in activities the child enjoys, while challenging them within that play to expand communication and interaction. For instance, if a child is lining up cars, the adult might join in and slowly introduce turn-taking or make the cars interact, thereby drawing the child into a shared world. The goal is to improve the child’s ability to relate, engage in back-and-forth interactions, and attend to emotional cues. Evidence for DIR/Floortime is still emerging: a few small studies have shown positive effects on parent–child interaction and the child’s social-emotional skills (for example, more spontaneous communication and longer periods of shared attention). However, results on language development and adaptive skills are less conclusive. Even so, many families and clinicians worldwide use play-based approaches as a complementary therapy. A case example: parents of a non-verbal 3-year-old implemented daily Floortime play sessions at home, focusing on simple games like peekaboo and chase. Over months, the child became more socially connected – smiling, making more eye contact, and using gestures to continue the play. While he still had delayed speech, his ability to engage socially improved, which later helped his progress in other therapies. Developmental approaches like this are often combined with ABA or speech therapy. They capitalize on intrinsic motivation (having fun) to help the child want to connect with others. Around the world, programs such as Play Project, Hanen’s “More Than Words,” and JASPER are variations of developmental play therapies. Parents report that these approaches can bring joyful interactions with their child and reduce the isolation that often comes with severe autism symptoms, even if they don’t rapidly accelerate language in the way structured therapies might. Overall, DIR/Floortime is considered a helpful intervention especially for improving the child’s social engagement and emotional reciprocity, and it works best when parents are extensively involved in daily play routines.
- Biomedical and Nutritional Interventions: Alongside behavioral and developmental therapies, many families explore biomedical interventions to address underlying health or metabolic issues that might exacerbate autism symptoms. These include dietary changes (detailed in the next section), nutritional supplements, and treating co-occurring medical conditions. For example, some children with ASD have gastrointestinal problems or food intolerances; treating those (through diet or medicine) can improve comfort and behavior. A popular approach worldwide is the gluten-free, casein-free (GFCF) diet, based on the theory that some autistic children can’t properly digest these proteins (found in wheat and dairy) and that peptides may affect the brain. While scientific studies on GFCF diets have had mixed results, a recent meta-analysis indicated that a GFCF diet might reduce certain autism symptoms like stereotyped behaviors and improve cognition in a subset of children. (Many of these studies are not double-blind, so more research is needed.) Apart from diets, parents and doctors sometimes try supplements such as omega-3 fatty acids (for brain development), vitamin B6 and magnesium (an older hypothesis for calming behavior), or melatonin for sleep issues. It’s important to note that no vitamin or supplement “cures” autism, but correcting any nutritional deficiencies or health issues can help the child be more receptive to other therapies. In medical settings, children are often screened for problems like iron deficiency, thyroid issues, or lead exposure, as addressing those can improve overall development. Some biomedical interventions target biochemistry – for instance, research has found that high-dose folinic acid (a form of folate) helped improve language in a subgroup of autistic children with certain folate autoantibodies (this is a specific population). Probiotics and other treatments for gut flora are also being studied, given the high prevalence of GI issues in ASD. Families should undertake biomedical changes under guidance of a health professional, especially diets (to ensure proper nutrition). In sum, biomedical interventions are adjuncts to therapy: by optimizing the child’s physical health and diet, we set the stage for better focus, sleep, and learning capacity, which can make behavioral and educational interventions more effective.
- Medications for Autism Symptoms: There is no medication that “cures” autism, but there are drugs that help manage certain symptoms or co-morbid behaviors. For a 3-year-old, medication is usually a last resort and used only for severe issues (since behavioral therapies are preferred in toddlers). However, by preschool age some autistic children exhibit dangerous levels of aggression, self-injury, or severe insomnia that impede any progress. In such cases, carefully prescribed medication can reduce these behaviors and improve the child’s ability to participate in therapy. Two medications are FDA-approved for autism-related irritability in children: Risperidone and Aripiprazole. Risperidone (an atypical antipsychotic) was the first approved drug for kids with autism, shown to significantly decrease aggression, self-harm, and severe tantrums in many children (in trials, nearly half of children on risperidone had major behavior improvement vs. far fewer on placebo). Aripiprazole (another antipsychotic) similarly has evidence of reducing irritability; one study found 52% of children on aripiprazole had a >25% reduction in irritability scores by 8 weeks, compared to 14% on placebo. These medications do come with side effects (weight gain, drowsiness, etc.), so doctors weigh the risks and benefits. For very young children, lower doses are used and monitoring is strict. Another common medication need is for sleep – many autistic toddlers have insomnia or night-wakings. Melatonin supplements (a hormone) are widely used and have a good safety profile; they often help regulate the child’s sleep cycle, which in turn improves daytime behavior and family well-being. Additionally, if a child has a co-diagnosis of ADHD (which can happen in ASD), stimulant medications might be tried around age 5 or 6 to help with focus – but at 3 years old, this is uncommon. Overall, medication in autism is about symptom management: for example, calming extreme behaviors so the child can learn in therapy, or treating epilepsy if present, or addressing anxiety. It’s always used in combination with educational and behavioral interventions, not as a standalone approach. Many families worldwide have seen that appropriate use of medication can be life-changing – for instance, one parent described how starting risperidone allowed their non-verbal 4-year-old to sit calmly and attend school, whereas before he was constantly in meltdown. In summary, while behavioral therapies remain the frontline treatment in early childhood, medications can play a supportive role for specific challenges.
- Parental Involvement and Success Stories: Across all interventions, one factor stands out in research: outcomes are best when therapy starts early and parents are actively involved. In fact, there are documented cases (often termed “optimal outcomes”) where children diagnosed with autism in early childhood no longer meet the criteria years later. These cases are rare but real. A longitudinal NIH-supported study followed a group of children who were diagnosed with autism before age 5 and received intensive early intervention; by the time they reached school age, a subset (~8-20% in various studies) had “lost” the autism diagnosis and were functioning indistinguishably from peers. Researchers confirmed these children truly had ASD early on (their initial symptoms, especially communication deficits and repetitive behaviors, were significant). Their dramatic improvement is often attributed to a combination of slightly milder symptoms to begin with, higher IQ, and extensive therapy and parental support. For example, one case report describes a boy diagnosed at 2½ who received 3 years of ABA, speech therapy, and OT with high family involvement; at 6, he was in a regular classroom with no support, indistinguishable from his peers in social and language abilities. While most autistic children will continue to have some level of disability, early and intensive intervention maximizes each child’s potential. Many parents around the world share success stories such as a child saying their first words after weeks of augmentative communication practice, or learning to point and share attention through play, or being able to tolerate new foods and expand their diet after sensory-focused feeding therapy. These improvements, big or small, are meaningful steps. As Dr. Thomas Insel of NIMH put it, autism outcomes vary widely, and “for an individual child, the outcome may be knowable only with time and after some years of intervention”. The consensus in the medical community is that high-quality early intervention optimizes outcomes. Even if a child doesn’t “outgrow” autism (which is uncommon), early therapy can often move them from severe autism (non-verbal, low engagement) to a much more functional place (using words, learning in school, etc.). This is hopeful news for parents: with therapies like those above, many 3-year-olds make significant strides. Autism is a lifelong neurodevelopmental condition, but children can and do improve, often considerably, with the right support. Hence, parents are encouraged to be proactive in seeking early diagnosis and comprehensive intervention – the earlier the start, the better the developmental trajectory.
Dietary Interventions in Autism Therapy
Dietary approaches have become a popular component of autism intervention plans. The idea is to adjust what the child eats (or doesn’t eat) to address possible food intolerances, nutritional deficiencies, or gut issues that might influence behavior and development. While diet changes are not a stand-alone cure for autism, some families report improvements in health and even in autism-related symptoms when certain foods are eliminated. Below is an overview of the most common dietary interventions, along with the foods excluded or included, and what evidence exists:
- Gluten-Free, Casein-Free (GFCF) Diet: This is by far the most well-known autism diet. It involves removing all gluten (a protein in wheat, barley, rye) and all casein (a protein in dairy products) from the child’s diet. In practice, that means no regular bread, pasta, cereal, or baked goods (unless made with gluten-free ingredients), and no cow’s milk, cheese, yogurt, ice cream, or other dairy. Families on a GFCF diet substitute with naturally gluten-free grains and starches (like rice, corn, oats, potatoes, quinoa) and dairy alternatives (such as almond milk, soy milk, or coconut yogurt). They ensure the child still gets protein through meats, eggs, beans, and non-gluten grains. The rationale behind GFCF is that some autistic children might have an underlying sensitivity to these proteins – there are hypotheses that peptides from gluten and casein may act like opioids in the brain or trigger inflammation, and that removing them could improve neurological function. Evidence: Scientific studies on GFCF diets have shown mixed results. A number of parent surveys and anecdotal reports claim benefits. For example, a UK survey found a majority of parents who tried GFCF noted improvements in their child’s bowel habits, overall health, sleep, concentration, and even social communication. Additionally, some older small-scale studies (Knivsberg et al. 2002, etc.) reported behavioral improvements on the diet. More recently, a systematic review (2022) of clinical trials found that across several studies, GFCF diet led to modest improvements in stereotyped behaviors and possibly cognition in some children. However, not all studies find a benefit – a rigorous 2010 trial by University of Rochester found no significant changes in autism symptoms with a GFCF diet (though that was a short-duration study). The consensus among experts is that GFCF diet may help a subset of children – particularly those with GI problems or suspected gluten/casein intolerance – but it’s not universally effective for all with ASD. Importantly, the diet must be done carefully: removing dairy can risk calcium and vitamin D deficiency, and removing gluten (which often also means less fortified grain intake) can risk B-vitamin and fiber deficiencies. Dietitians warn that if a child already has a very limited diet (common in autism due to picky eating), cutting out major food groups can cause weight loss or poor growth. In the UK, the National Autistic Society notes that while some report feeling better on GFCF, there isn’t enough evidence to recommend it for everyone, and NICE guidelines advise against exclusion diets for core autism treatment. The bottom line: GFCF is something families might trial (ideally with medical/dietetic supervision) for a few months to see if it helps, especially if the child has chronic digestive issues. Some children who are found to have true gluten intolerance (celiac disease) or milk protein allergy definitely benefit from removal. For others, it may not make a difference. Any positive response tends to be observable within 3-6 months if it’s going to occur.
- Other Dietary Strategies: Aside from GFCF, families explore various other diet modifications:
- Allergen-Free or Anti-Additive Diets: Some parents eliminate artificial food colorings, preservatives, and high-sugar foods (thinking these might worsen hyperactivity or behavior). This is similar to the Feingold diet used in ADHD. While not specific to autism, a generally healthy diet with limited processed foods is often recommended for overall well-being.
- Specific Carbohydrate Diet (SCD): This diet removes complex carbohydrates and sugars, allowing only certain fruits, honey, and well-cooked carbs (aiming to alter gut bacteria and reduce GI issues). It’s more restrictive than GFCF and has mainly anecdotal support.
- Ketogenic or Modified Atkins Diet: In a few cases where autism overlaps with epilepsy, a ketogenic (high-fat, very low-carb) diet might be used to control seizures. Interestingly, some studies have noted mild improvements in autistic behaviors on a keto diet, but it’s not widely used for autism alone due to its difficulty.
- Supplements and Nutrition: Ensuring adequate omega-3 fatty acids (from fish or flaxseed) has been researched because omega-3s are important for brain development. Some trials of fish oil supplements in autistic children showed improvements in social eye contact and reduction in hyperactivity, though findings are not uniform. Likewise, vitamin D supplementation is studied, as low vitamin D levels have been observed in some children with autism. If a child is a very picky eater, a pediatric multivitamin is often given to cover basic nutrients. Probiotic supplements are another popular intervention aimed at improving gut health, under the theory that gut microbiome imbalances could influence behavior. While there is early research hinting at microbiome’s role, it’s still experimental.
- Casein-free but not Gluten-free, or vice versa: Some families find only dairy seems problematic for their child (perhaps causing loose stools or eczema), so they remove dairy alone. Others suspect only gluten/wheat is an issue and remove that alone. The interventions can be tailored to the child’s suspected triggers or tested via elimination diets. If a child has noticeably adverse reactions to certain foods (e.g. gets hyperactive after a sugary snack or gets stomach pain after milk), those foods can be reduced or replaced.
part 3 : What can be the most mis diagnosis with Autism : Receptive Language Disorder (RLD)
Scientific Studies on Receptive Language Disorder (RLD) vs. ASD
- Language Profiles: Research shows toddlers with primary language disorder differ markedly from those with autism. For example, when matched on expressive language level, children with developmental language disorder (DLD/RLD) had better nonverbal cognition, more pretend play and gesture use, and stronger responses to language than age-mates with ASD. By contrast, ASD toddlers showed poorer gaze, social sharing, and back-and-forth communication, even when expressive vocabulary was similar. In one study, ASD children had relatively more receptive (comprehension) deficits while DLD (language disorder) children had more expressive deficits. These differences help clinicians distinguish RLD (children mainly struggling to understand language but socially engaged) from ASD (children with prominent social-communication and behavioral deficits).
- Diagnostic Criteria: In current nosology, RLD falls under “Language Disorder” or “Developmental Language Disorder” (DLD). By definition this excludes ASD: language deficits in DLD are not caused by autism or other known conditions. DSM-5 requires ASD to have pervasive social-communication deficits plus restricted interests/behaviors. In practice, RLD patients lack ASD’s hallmark features (they make good eye contact, engage in pretend play, share affect, etc.) even if they cannot follow directions or answer questions well.
- Longitudinal Outcomes: Follow-up studies indicate severe RLD often persists. A Scottish cohort of 58 children with severe receptive SLI (language impairment) showed that by school age only ~3% had normal comprehension scores, despite normal IQs. In that study two-thirds still had significant language impairments, and virtually all had severe expressive deficits as well. Family studies found that about one-third of “unaffected” siblings had subtle language weaknesses, reflecting genetic risk. The authors conclude RLD has a poor prognosis without intervention, and recommend early identification and therapy.
Case Reports and Published Accounts
- Al’s Case (Malaysia, 2023): A recent case report described a young boy (“Al”, preschool age) evaluated for ASD but ultimately diagnosed with language disorder. He scored below the autism cutoff on screening scales, and his cognitive and adaptive profiles were inconsistent with typical ASD but matched DLD. After comprehensive testing, clinicians reclassified him with a language disorder. The authors emphasize that careful, evidence-based assessment (examining language comprehension, cognition and behavior) is critical to avoid misdiagnosis.
- Classic Studies: Earlier comparative studies (e.g. Bartak et al. 1977) similarly found overlaps and distinctions between ASD and “specific developmental receptive language disorder” (an old term). In general, these studies noted that RLD children have severe receptive (and often expressive) deficits but lack the social deficits of autism. (See reviews of Bartak et al. in Rhea Paul 2008.)
Parent and Real-World Stories
- Anecdotal Reports: Some parents report trajectories matching RLD rather than autism. For example, the Cherab Foundation (a non-profit for speech disorders) published a story of one mother who gave her 3-year-old (diagnosed with severe speech/language delay) a daily fish oil supplement. Within weeks “his vocabulary exploded,” she said. The foundation also cited small trials where children (ages 2–8) with speech disorders showed dramatic improvement (in speech, behavior, eye contact) after omega-3/6 supplementation. While these are anecdotal, they illustrate that families often explore nutritional aids.
- Online Community: On forums and blogs, some parents describe children once thought to be “severely autistic” who later were found to have only language comprehension issues. These reports emphasize scenarios like a 2–3 year-old not talking or responding to name but reacting socially once language therapy began. (Such accounts are informal, but parents stress differences like rapid gains in play and social smiling once nonverbal language skills improve.)
Therapy and Intervention Strategies
- Speech and Language Therapy: Early, intensive language intervention is the mainstay. Best practice involves 1:1 speech therapy focusing on comprehension (following simple instructions, answering questions) as well as expressive skills. For example, in one controlled trial children received 45-minute sessions 3×/week along with parental training. A Cochrane review noted that while more research is needed on treating receptive deficits, therapies show clear gains in expressive language. In practice, therapists use play-based and naturalistic methods (Hanen, play therapy, modeling) rather than autism-specific methods. Crucially, caregivers are coached to use clear, slow speech and visual cues (gestures, pictures) to boost understanding. A pediatric neurology brief notes that early diagnosis and intervention are strongly recommended for RLD.
- Enhanced Speech Input: Research by Tallal and colleagues has shown that altering speech acoustics can help comprehension. In “fast-for-word” programs, rapid speech sounds are slowed and emphasized. Compared to natural speech, this acoustically modified training significantly improved receptive language in children with language impairment. Such evidence-based programs (or software apps based on them) may be used adjunctively.
- Addressing Social Skills: Unlike ASD, children with RLD usually have age-appropriate social interest, so therapy does not focus on social deficits. However, therapists may still support pragmatic skills (turn-taking, eye contact) as language emerges. Behavioral interventions like ABA are not typically indicated unless autism features truly emerge. Instead, families often use structured language enrichment and responsive interaction strategies.
Dietary and Nutritional Interventions
- Omega-3/6 Fatty Acids: Several studies suggest possible benefit of essential fatty acids in language delay. In one Egyptian trial, preschoolers with specific language impairment who received daily omega-3 supplements (EPA/DHA) plus speech therapy made significantly greater language gains than those with therapy alone. The authors concluded that “PUFA supplementation has a beneficial role in the management of specific language impairment along with speech therapy”. In a small trial of toddlers at risk for ASD (many with language delay), a 3-month omega-3/-6 regimen led to greater increases in communicative gestures versus placebo.
- Anecdotal Dietary Changes: Some parents of language-delayed children try special diets. For instance, the Cherab Foundation report mentions a mother whose son improved after fish-oil capsules. Others consider gluten- and casein-free diets (common in autism communities), though scientific support is weak. Importantly, no conventional “diet cure” exists for RLD: clinicians emphasize balanced nutrition and treating any medical issues (hearing, digestion, etc.) that might affect communication.
- Other Supplements: Beyond EFAs, there is little evidence for vitamins or herbs in RLD. Families should be cautious: for example, broad nutritional counseling (adequate protein, vitamins) may support overall development, but restrictive or unproven supplements (megadoses, “detox” diets) are not recommended without medical supervision.
Part 4 : How AI can Help ?
How AI Is Transforming Diagnosis and Therapy for Childhood Language Disorders and Autism
Diagnosing conditions like Receptive Language Disorder (RLD), developmental language delays, or autism spectrum disorder in young children can be challenging. Many early signs are subtle – a toddler might struggle to understand words, or an autistic child’s social cues might be hard to quantify – and specialists are in short supply. Early intervention is crucial, but families often face long waits for evaluations. In recent years, artificial intelligence (AI) and deep learning have emerged as powerful tools to support both early diagnosis and therapy in this arena. From smartphone apps that analyze a toddler’s gaze and babbling, to game-like platforms that keep kids engaged in practicing language skills, AI is helping clinicians and families detect issues sooner and personalize treatment. Below, we explore current and emerging AI-driven technologies – with real-world examples – and their practical impact on children with language disorders or autism.
AI for Early Diagnosis and Screening
1. AI Video and Gaze Analysis: New AI tools can pick up behavioral clues from video that humans might miss. For example, Cognoa’s Canvas Dx is an FDA-cleared system that analyzes short home videos of a child’s behavior, along with caregiver questionnaires, to help doctors diagnose autism in children as young as 18 months. Another system, EarliPoint by EarliTec, uses eye-tracking: toddlers watch brief videos while the system tracks their eye movements. AI then detects subtle deviations in gaze patterns – such as missing social cues on screen – that are strong indicators of autism risk. These video-based analyses provide objective data, which can lead to earlier and more accessible screenings than traditional observations.
2. AI Speech Pattern Recognition: Many researchers are leveraging deep learning to analyze children’s speech for diagnostic insights. Some autistic children, for instance, have distinct vocal patterns (such as unusual pitch, intonation, or taking fewer turns in conversation). A deep-learning algorithm called ASDSpeech was trained on recordings of autistic kids during play sessions and can identify such speech features that correlate with the child’s social-communication abilities. Earlier tools like the LENA recorder (a wearable audio device) similarly tried to spot unusual speech patterns in a child’s home environment, but modern AI is more powerful. In one study, an AI system developed at MIT was able to analyze a few minutes of a child’s speech (from casual conversation or storytelling) and accurately flag potential language disorders – achieving high accuracy in identifying children with developmental language disorder vs. typical peers. By automating speech analysis, AI can catch subtle signs of RLD or other language delays that might be overlooked, especially in kids who are quiet or masking their difficulties.
3. Behavioral Screening Apps: Beyond single indicators, some cutting-edge apps look at multiple behaviors at once. Researchers at Duke University, for example, have created a tablet-based app called SenseToKnow that in just 10 minutes screens a child for autism by measuring a variety of behaviors. As the child engages with games on the tablet, the app’s AI is simultaneously tracking facial expressions, eye gaze, head movements, and even the child’s fine motor skills during a bubble-popping game. All these data points are weighed to predict the likelihood that the child is on the autism spectrum. Importantly, the system doesn’t just give a binary result – it provides an interpretable report of which specific behavioral clues (e.g. limited eye contact or slow motor response) led to its conclusion. This transparency helps clinicians and parents trust the AI’s findings and know what to look into further. Because it only requires a common tablet, such an app can be used in a pediatrician’s office or even at home, bringing early screening to families who may not have specialized centers nearby.
4. Analyzing Infant Signals: Looking even earlier in development, scientists are exploring whether AI can find warning signs in infants. One fascinating line of research examines baby cries. A recent review found that acoustic features of an infant’s cry – such as pitch (fundamental frequency), duration, and voice quality – show measurable differences in babies who later are diagnosed with autism. Using machine learning to analyze cry recordings, researchers have identified patterns that could act as early vocal biomarkers of neurodevelopmental issues. While this work is still preliminary, it suggests future AI tools might literally “listen” for early signs of developmental disorders long before a child can speak. Imagine a smart baby monitor that could alert parents and doctors to atypical cry patterns – offering a non-invasive, objective cue to investigate a child’s development further. Such AI-driven early warning systems could lead to evaluations for conditions like autism or language delays at a very young age, when interventions might have the greatest impact.
AI-Powered Tools for Language Therapy and Intervention
1. Gamified Speech Therapy: Getting young children to participate in traditional speech therapy can be tough – it’s hard to repeat syllables or sounds over and over when it feels like work. AI is helping to gamify this process. For example, a platform called TikTalk turns speech therapy exercises into a video game experience. A child might help an on-screen character navigate an adventure by speaking target words or sounds correctly. Behind the scenes, TikTalk’s AI listens to the child’s pronunciation via the device microphone. It gives immediate feedback, and the game rewards progress, motivating kids to practice longer. The app is customizable by speech-language pathologists (SLPs): therapists can select specific words or sounds for the child to focus on, and the AI will analyze the child’s attempts, track their accuracy, and even adjust the game’s difficulty or hints in real-time. This means practice can happen at home in between clinic visits – a boon for busy families – and the therapist gets detailed data on how the child did, enabling them to fine-tune the next session’s plan remotely. By making therapy fun and adaptive, AI gamification helps children practice more often and more effectively.
2. At-Home Speech Coaching Apps: Beyond games, there are also simple mobile apps acting as AI speech coaches for kids with speech delays. One example is Huni, a speech-training app designed for children who are late talkers or have conditions like apraxia or autism. Huni uses AI-based speech recognition to engage the child in a guided practice: the app displays a word (with a picture) and prompts the child to say it aloud. If the child’s pronunciation is correct, the app acknowledges it (for instance, with a fun animation or a cheer); if not, it encourages them to try again, and the AI can highlight the parts of the word that were mispronounced. In essence, it’s like a personalized, always-available speech therapist that provides instant feedback. The content is kid-friendly – Huni includes illustrated word packs (family, food, animals, etc.) to build useful vocabulary while keeping the child’s interest. For a child who is non-verbal or minimally verbal, just getting them to attempt sounds in a playful context can be a big step, and parents can use such apps daily to supplement professional therapy.
3. Interactive Language Games: Several startups have created interactive language-learning apps for children with developmental language disorders. Platforms like Speech Blubs and Otsimo (popular with many families of children with delays) use AI to personalize the learning experience. These apps often work by showing the child a short video or an interactive prompt – for example, a video of another child pronouncing a word, or a prompt like “find the cat” with pictures. The child then responds, either verbally or by selecting an answer, and the app’s AI processes that response. Speech recognition is used to check if a word was said correctly, and the app might give praise (“Great job!”) or a correction (“Oops, try again, say ‘ca-t’”). Some apps even use the front camera to implement augmented reality filters – for instance, putting funny hats or animal ears on the child’s face while they practice certain sounds, turning speech practice into a sort of Snapchat-like game. The AI in these apps can adjust to each user: it might simplify tasks if the child is struggling, or introduce longer phrases as they improve. By combining animation, feedback, and adaptive challenge, these AI-driven games hold a child’s attention far better than flashcards or drills, which leads to more frequent practice and gradual improvement in language skills.
4. Social Robots as Therapy Aides: Another innovative application of AI in intervention is social robots. Children on the autism spectrum, in particular, can sometimes find interactive robots more engaging or less stressful than human strangers, making robots ideal therapy buddies. One example is the QTrobot – a child-sized humanoid robot with a friendly face and programmable AI routines. Therapists have used QTrobot to help autistic children with both communication and emotional skills. In a receptive language exercise (understanding words), the robot might say, “Can you find the apple?” while showing a few objects or images. If the child correctly identifies the apple, the robot’s AI recognizes that success (via camera vision or the child’s touch on a tablet) and the robot might do a happy dance or give praise, making the child smile. If the child is unsure, the robot can give a hint or repeat the prompt. The advantage is that the robot delivers these prompts in a very consistent, patient manner, and can exaggerate its gestures or facial expressions to keep the child’s attention. Long-term studies of robot-assisted therapy have reported improvements in autistic children’s engagement and language comprehension – in part because the novelty and predictability of the robot can reduce anxiety and encourage kids to respond more often. While still an emerging field, robot-mediated intervention shows how AI can literally step into the room with a child and augment the work of human therapists.
5. Augmented Reality for Social & Language Skills: Emerging technologies like augmented reality (AR) and virtual reality (VR) are also being tested to support kids with language and social communication challenges. For example, researchers have built AR games where a child wears a device (or uses a tablet camera) and sees virtual characters or objects overlaid on the real world. The AI might then guide the child through tasks like “Help the bunny find the red circle” – which requires the child to understand the instruction, look around to spot the virtual red circle in their environment, and maybe say “I found it!” to confirm. This kind of immersive play can be especially helpful for practicing concepts like following directions or turn-taking in conversation. Early pilot programs using AR/VR for children with DLD and autism have shown positive engagement, and importantly the AI can log how the child interacts – e.g., did they respond to a prompt, how long did it take – giving therapists data on the child’s performance in a simulated real-world scenario. In the near future, a home-based AR app could have a child practice listening and speaking in a virtual playground or classroom, safely preparing them for real-life interactions. AI ensures the experience adapts to the child’s level: if they get things right easily, it gets a bit harder; if they struggle, it provides more clues or repeats, all in a way that feels like play, not a test.
A toddler uses the SenseToKnow tablet app, which employs AI to analyze multiple behaviors (facial expressions, eye gaze, motor responses) during gameplay for autism screening. Such apps enable earlier, home-based evaluations – helping families get timely insights and guiding clinicians with automated observations. The on-screen bubbles in this game measure the child’s motor skills and attention while other sensors track eye contact and expressions.
Personalized Therapy and Remote Support Through AI
One of AI’s biggest strengths is personalization. Every child with a language disorder or autism has a unique profile of strengths and needs. AI tools can crunch huge amounts of data from a child’s interactions – whether it’s weeks of practice scores from a speech app, or hours of classroom video – to tailor support for that individual. This means therapy can move away from a one-size-fits-all workbook and become more responsive. For example, an AI-based coaching system might notice that a particular child consistently pronounces “k” sounds incorrectly at the ends of words, but does fine with “s” sounds. The system could then suggest to the therapist to prioritize exercises on words like “book” and “duck” before tackling other sounds. Or in the context of autism, if a child using an AI-assisted learning program shows better engagement with visual puzzles than with listening tasks, the AI can recommend using more visual supports in their learning plan.
Another advantage is remote monitoring and support. In between formal therapy sessions or evaluations, a lot can happen – or not happen – in a child’s progress. Traditionally, therapists rely on parents to report how practice at home went, or teachers to share observations from class, which can be subjective or hard to collect systematically. AI can fill this gap by continuously (and discreetly) observing and analyzing. For instance, the National AI Institute for Exceptional Education (a U.S. initiative) is developing classroom observation tools that use cameras and microphones (with privacy safeguards) to monitor children’s interactions. The AI might pick up that one child in a preschool class rarely responds when the teacher asks questions or often has a blank expression during story time. It would compile these observations into a weekly summary for the teacher, highlighting patterns that suggest a possible receptive language issue or hearing problem. With that prompt, the teacher can engage the school’s speech-language pathologist to evaluate the child sooner rather than later. Similarly, for a child already in therapy, an AI could track therapy sessions (even via telehealth videos) and measure things like the child’s eye contact, the latency of their responses, or their emotion on their face over time – providing the clinician with objective progress metrics.
For families, especially those in remote areas or with limited services, these AI tools offer more autonomy and support. Rather than waiting months on a waitlist, parents can use an AI screening app to get an initial read on their child’s development and decide if they should travel to see a specialist. During therapy, if in-person sessions are infrequent, an AI app or game ensures the child still gets daily practice in a guided way, and parents get tips on how to help. This at-home practice is reinforced by the fact that the therapist can often review the app’s data: for example, see which words the child struggled with or how often they used the app that week. It creates a feedback loop where the family and clinician stay connected via data, making the therapy more consistent and effective.
For clinicians, AI is becoming a valuable assistant. It can handle time-consuming tasks like transcribing a child’s speech samples and scoring them against developmental norms, or analyzing hours of behavior to quantify things like “initiations of joint attention” (a key social metric in autism). By automating these analyses, AI frees specialists to spend more time working directly with children and planning interventions, rather than laboring over paperwork or video coding. Moreover, AI can surface insights that inform treatment plans – essentially acting as a second pair of eyes. One clinician described an AI tool as being able to “see the forest for the trees” in a complex case: by aggregating data, it might reveal that a child’s language comprehension is much better in one-on-one settings than in groups, suggesting that part of the child’s issue is auditory distraction or social anxiety rather than purely language deficit. That kind of insight could lead to a tailored therapy approach (maybe starting in quiet environments, then gradually adding background noise or peers). In this way, AI helps ensure therapy is personalized to the child’s specific profile, not just based on broad diagnosis.
It’s important to note that AI is not replacing human therapists or doctors – rather, it’s augmenting their capabilities. The empathy, creativity, and expertise of clinicians remain central, but AI provides them with richer information and tools to work smarter. Think of AI as giving clinicians “data superpowers,” allowing them to detect patterns or measure progress in ways that would be impractical manually. Families, on the other hand, gain empowerment through knowledge – an informed parent equipped with an app that tracks their child’s vocabulary growth, for instance, can make better decisions and feel more engaged in the therapeutic process. Ultimately, the collaboration between human and artificial intelligence is leading to more proactive care: issues are spotted earlier, and interventions can be started sooner and tuned more precisely to each child’s needs.
Real-World Impact and Future Outlook
AI-driven diagnostic and therapy tools are already having a real-world impact for many families. They are shortening the path to diagnosis – for example, instead of spending six months on waiting lists and evaluations, parents have been able to use apps like Cognoa or SenseToKnow to get an indication within days or even minutes, then fast-track their child to appropriate specialists. This earlier identification can mean children with autism or language disorders start receiving help at 2 or 3 years old instead of 5 or 6, which, as research shows, can greatly improve developmental outcomes. AI is also expanding access: a family in a rural area might not have any certified speech therapists nearby, but they can still engage their child with a speech practice app or do an AI-guided screening over a smartphone. For many, these technologies reduce the feeling of helplessness during the “wait and see” period – parents can actively do something constructive and track progress.
For healthcare providers and educators, AI tools offer a way to scale up services and maintain quality. An algorithm doesn’t get tired or biased, so it can, for instance, analyze every vocalization a child makes in a 30-minute play session without missing any, something even the best clinician would struggle to do by ear. This consistency means subtle signs, like a very limited range of different words used by a 3-year-old, are less likely to be overlooked. In practice, we are seeing more pediatric clinics adopt “digital phenotyping” tools – essentially apps or devices that collect developmental data – as part of routine check-ups. Early studies find that these AI assessments often agree with specialist evaluations, and in some cases catch red flags that lead to referrals which otherwise might not have happened. Schools, too, are experimenting with AI to support special education: a pilot program might use a camera in the lunchroom to identify a child who never interacts with peers (potentially due to a social communication disorder), prompting gentle intervention. All of this leads to more data-driven, timely decision-making in care.
Looking ahead, the next frontier is making these AI tools even more accurate, interpretable, and integrated into care. Researchers are working on training AI models with multimodal data – not just one type of input, but combinations like video + audio + wearable sensor data. For example, an autism detection algorithm might combine facial analysis, voice tone analysis, and heart rate or movement data from a smartwatch to paint a fuller picture of a child’s behavior. By fusing inputs, AI may be able to detect complex patterns (maybe a certain gesture combined with a certain vocal intonation) that single-modality tools would miss. Efforts like the Duke project and others are showing that using “all the sensors” can improve screening accuracy and also make the AI’s confidence more reliable. We can also expect AI to become more explainable. Clinicians and families are more likely to trust an AI’s recommendation if it comes with a clear rationale – e.g., “the system flagged language delay because your child’s spoken sentences were on average only 2 words long, which is below age expectations.” Future apps will likely provide these kind of explanations automatically (some already do, as noted with interpretable outputs identifying which behaviors mattered). This not only builds trust, but also educates parents on what to watch for in their child’s daily life.
Privacy and ethics are being taken seriously as well. Developers understand that analyzing a child’s speech or video involves sensitive data. Newer AI applications are starting to perform more processing directly on your device (on-device AI) or using encryption, so that a child’s recordings aren’t exposed unnecessarily. Policies and guidelines are emerging to govern how AI is used in diagnostics – for instance, ensuring that these tools are validated across diverse populations so they work equally well for different genders, ethnicities, and languages. The FDA in the US is now evaluating AI medical devices like any other medical tool, which adds a layer of oversight and assurance of safety/effectiveness.
In summary, AI and deep learning are becoming invaluable allies in the journey from identifying a child’s communication challenges to delivering effective help. Five years ago, the idea that a smartphone app could suggest your toddler might have autism, or that a cute robot could help your child learn new words, seemed like science fiction – now it’s a reality supported by growing evidence. Families are finding these tech tools can reduce uncertainty and provide personalized support 24/7, in ways that nicely complement what doctors and therapists do. Clinicians, for their part, are harnessing AI to enhance their assessments and to reach children who might otherwise fall through the cracks. There’s still much to learn and perfect, but the trajectory is clear: AI is making the process of diagnosing and treating RLD, language delays, and autism more efficient, more accessible, and often more engaging for the children themselves. For any parent anxious about their child’s development, that’s good news – it means more resources and hope are available today than ever before, powered by innovations at the intersection of technology and child healthcare.
Sources: Recent advances and examples have been drawn from a range of research studies, clinical trials, and tech innovations in 2023-2025. Key references include FDA-cleared AI diagnostic tools for autism, academic projects like Duke’s multi-behavior screening app, speech analysis research from autism clinics, and reports on AI-driven therapy platforms in use by speech therapists, among others, as cited throughout this article. These illustrate the tangible impact AI is having right now on early identification and intervention for children with communication disorders.